Obstetric anaemia toolkit
This toolkit is for midwives and obstetricians to help implement good practice within hospital and community settings.
It provides a pathway to identify, diagnose and treat iron deficiency anaemia during pregnancy and the postpartum period. It demonstrates how patient blood management initiatives can help prevent iron deficiency and iron deficiency anaemia from occurring.
The resources in this toolkit are for you to edit and use in your practice. Please acknowledge the Patient Blood Management England Obstetric Anaemia Project when you use them.
In this section
Pages in the 'Identify and manage anaemia' section
About obstetric anaemia
 The British Society for Haematology identifies obstetric anaemia as a haemoglobin level of:
The British Society for Haematology identifies obstetric anaemia as a haemoglobin level of:
- less than 110 g/L during the first trimester
- less than 105 g/L during the second and third trimester
- less than 100 g/L postpartum
Obstetric anaemia can cause extreme fatigue and increase the risk of infection, postpartum haemorrhage and depression.
In neonates, it can increase the risk of low birth weight, impaired cognitive function and iron deficiency anaemia.
How patient blood management helps
A World Health Organisation (WHO) policy brief in 2017 urged health care providers to implement patient blood management initiatives to minimise the negative impact of anaemia on pregnant women and people, and on neonates.
This toolkit supports the global initiative to reduce obstetric anaemia by 50% by 2025.
In the UK, this equates to a reduction from just under 25% of the pregnant population to around 12%.
Infographics
These infographics are designed for you to use alongside appropriate text in presentations and educational resources. Please acknowledge the NHS Blood and Transplant Patient Blood Management team as the author.
Iron deficiency anaemia
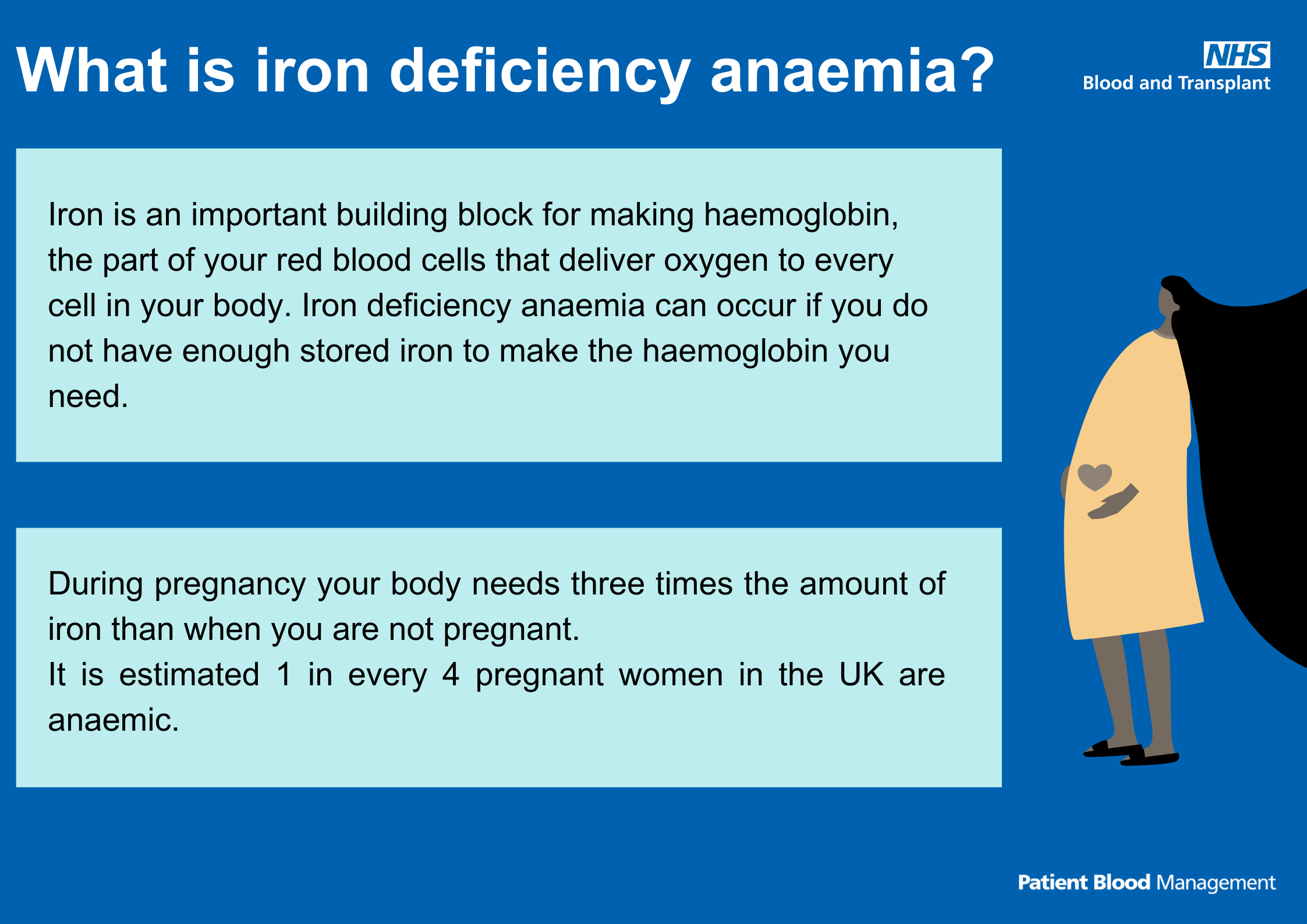
Text reads: "What is iron deficiency anaemia?
Iron is an important building block for making haemoglobin, the part of your red blood cells that deliver oxygen to every cell in your body. Iron deficiency anaemia can occur if you do not have enough stored iron to make the haemoglobin you need.
During pregnancy your body needs three times the amount of iron than when you are not pregnant.
It is estimated 1 in every 4 pregnant women in the UK are anaemic."
How will I know if I am anaemic?
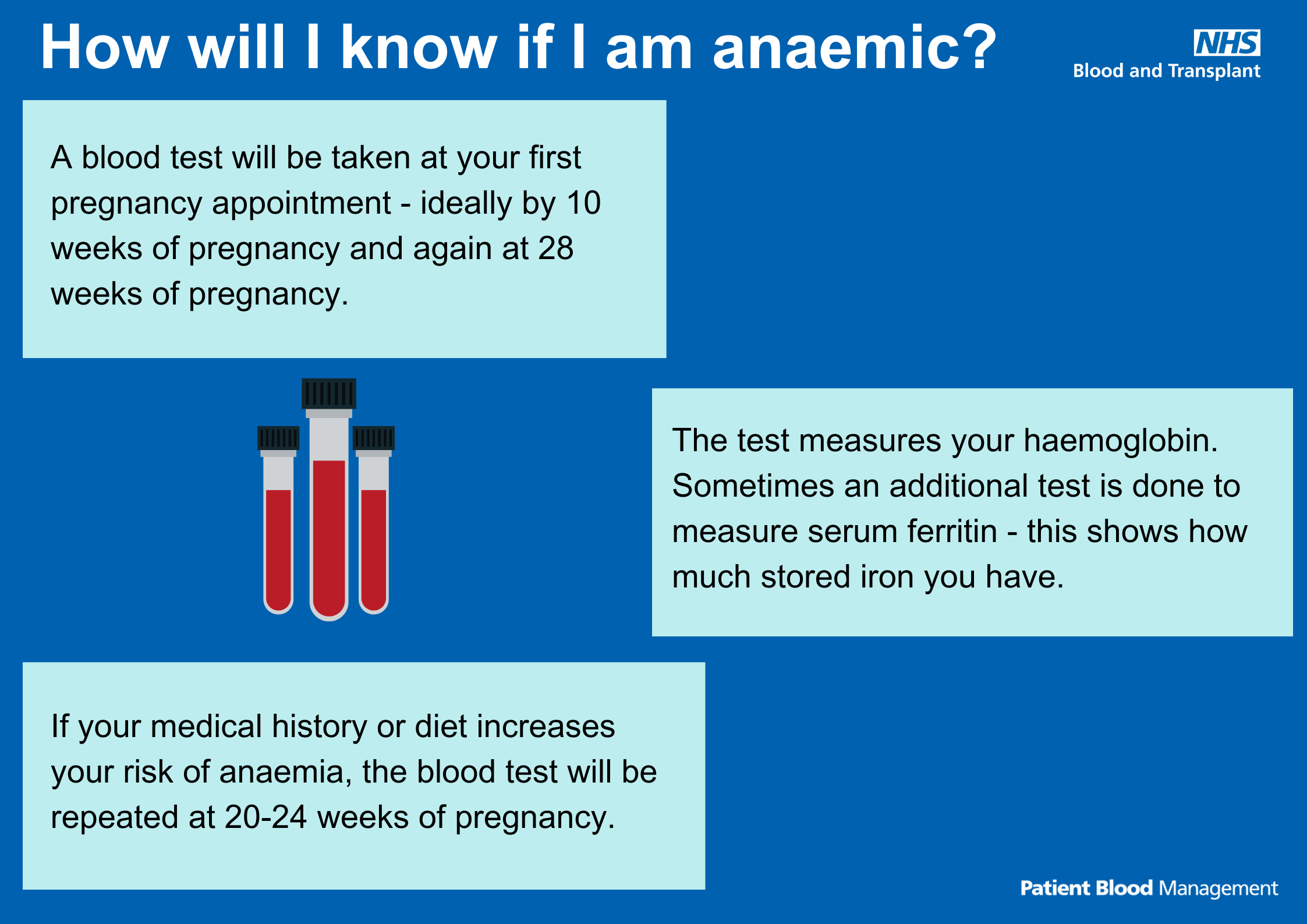
Text reads: "How will I know if I am anaemic?
A blood test will be taken at your first pregnancy appointment – ideally by 10 weeks of pregnancy and again at 28 weeks of pregnancy.
The test measures your haemoglobin. Sometimes an additional test is done to measure serum ferritin – this shows how much stored iron you have.
If your medical history or diet increases your risk of anaemia, the blood test will be repeated at 20-24 weeks of pregnancy."
How can anaemia make you feel?
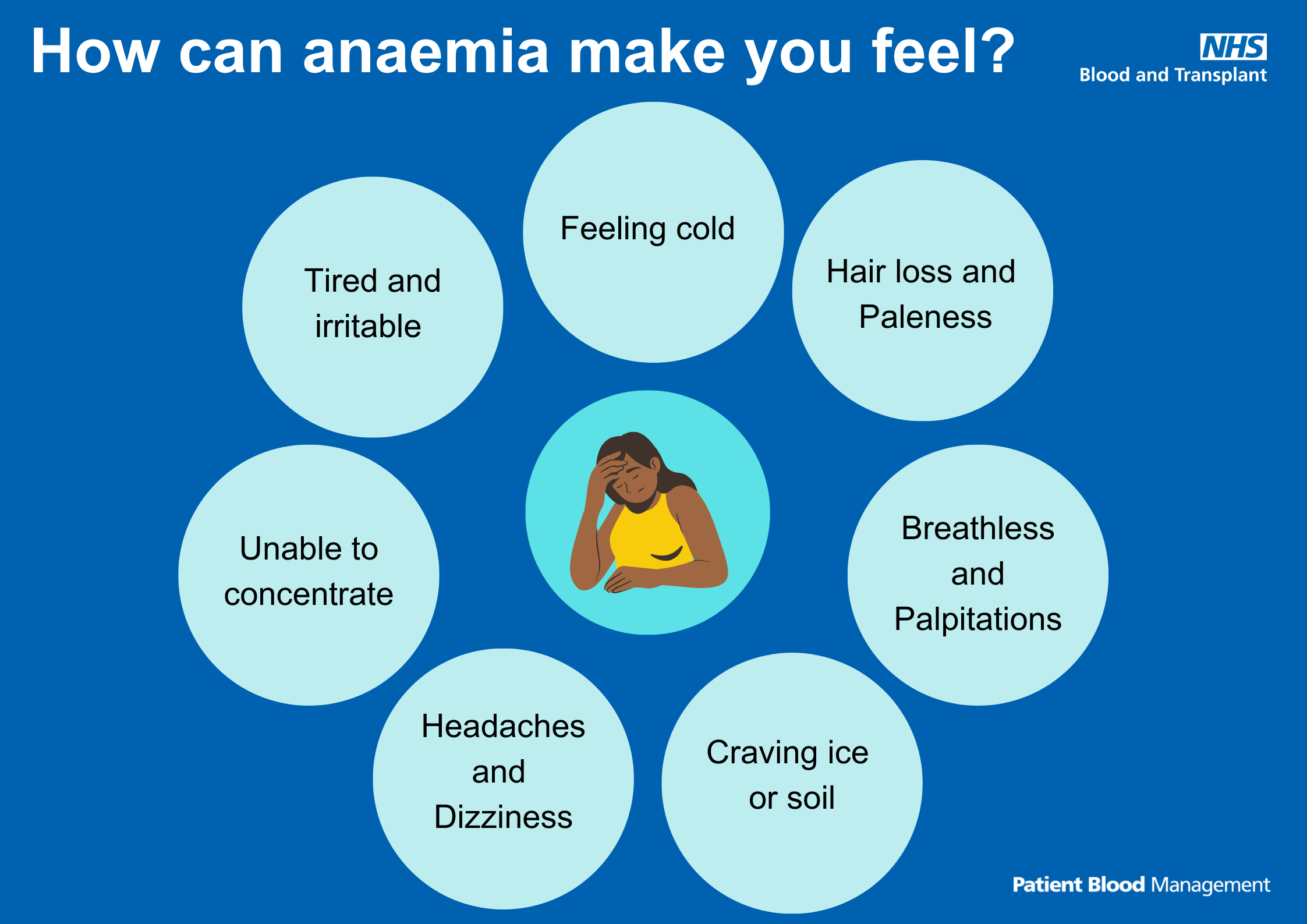
Text reads: "How can anaemia make you feel?
- Feeling cold
- Hair loss and paleness
- Breathless and palpitations
- Craving ice or soil
- Headaches and dizziness
- Unable to concentrate
- Tired and irritable"
Risks to mother and baby
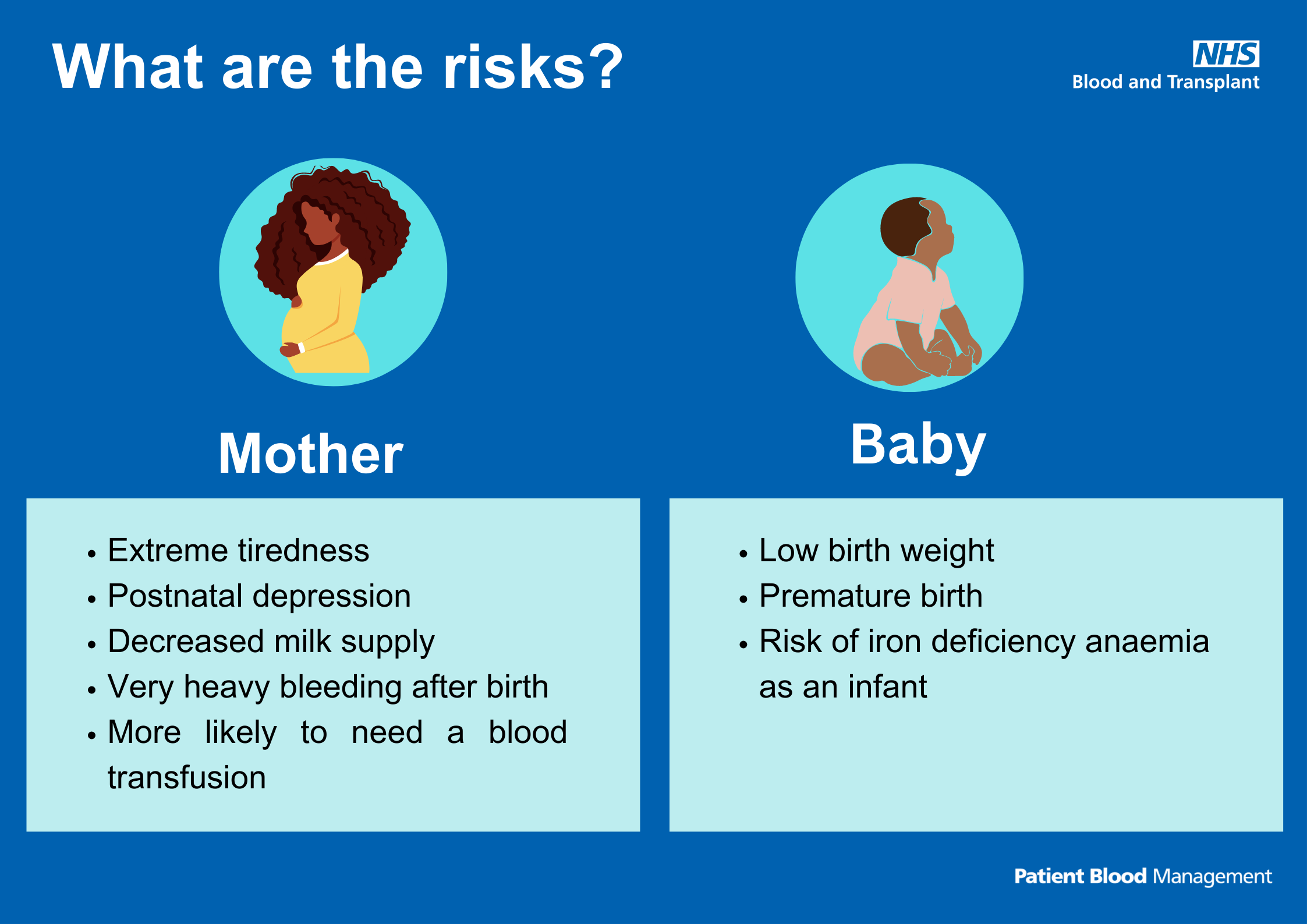
Text reads: "What are the risks?
Mother:
- Extreme tiredness
- Postnatal depression
- Decreased milk supply
- Very heavy bleeding after birth
- More likely to need a blood transfusion.
Baby:
- Low birth weight
- Premature birth
- Risk of iron deficiency anaemia as an infant"
Download the risks to mother and baby infographic (PDF 85KB)
How can I prevent anaemia?
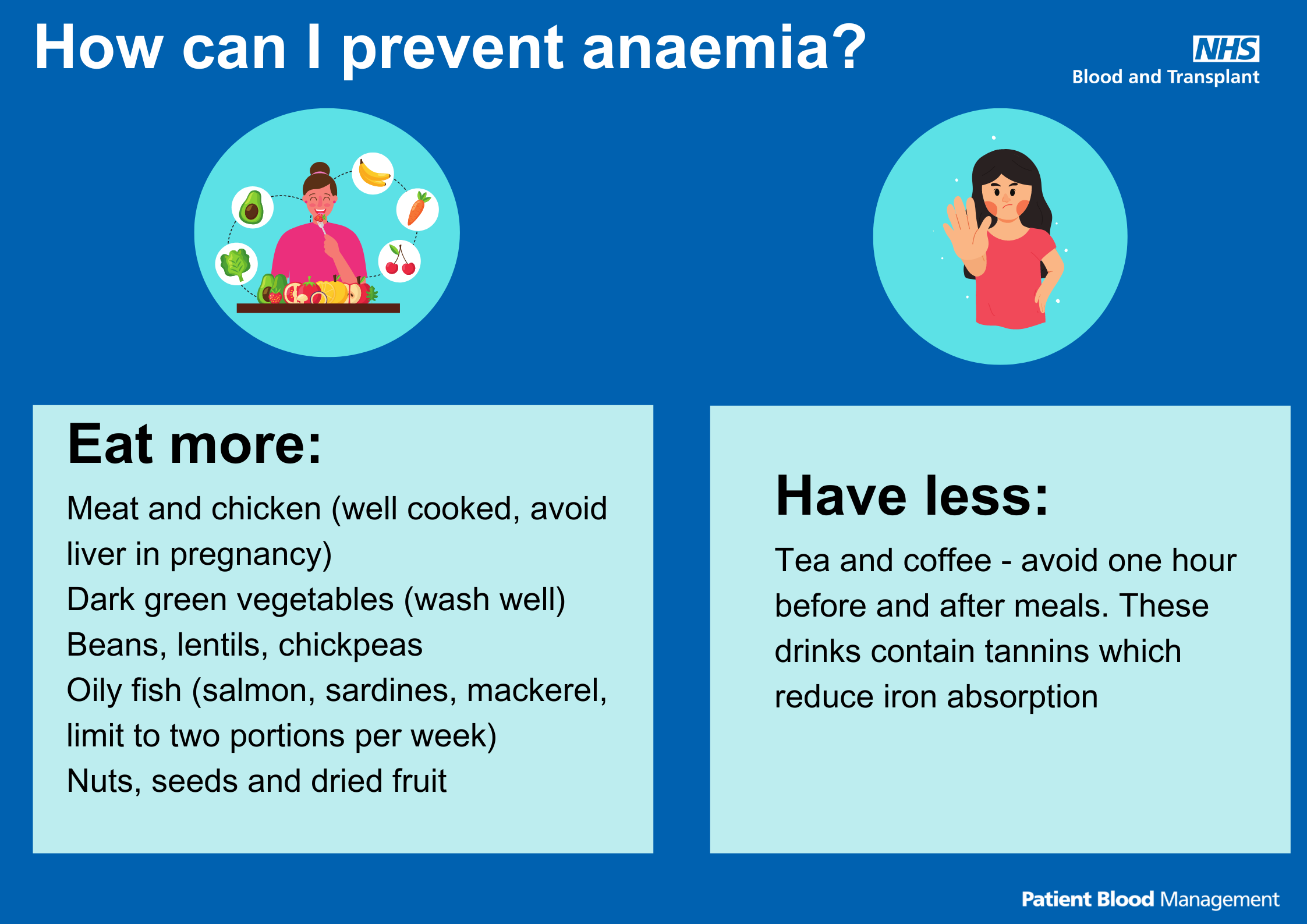
Text reads: "How can I prevent anaemia?
Eat more:
- Meat and chicken (well cooked, avoid liver in pregnancy)
- Dark green vegetables (wash well)
- Beans
- Lentils
- Chickpeas
- Oily fish (salmon, sardines, mackerel, limit to two portions per week)
- Nuts, seeds and dried fruit
Have less:
- Tea and coffee - avoid one hour before and after meals. These drinks contain tannins which reduce iron absorption"
Iron deficiency anaemia risk factors
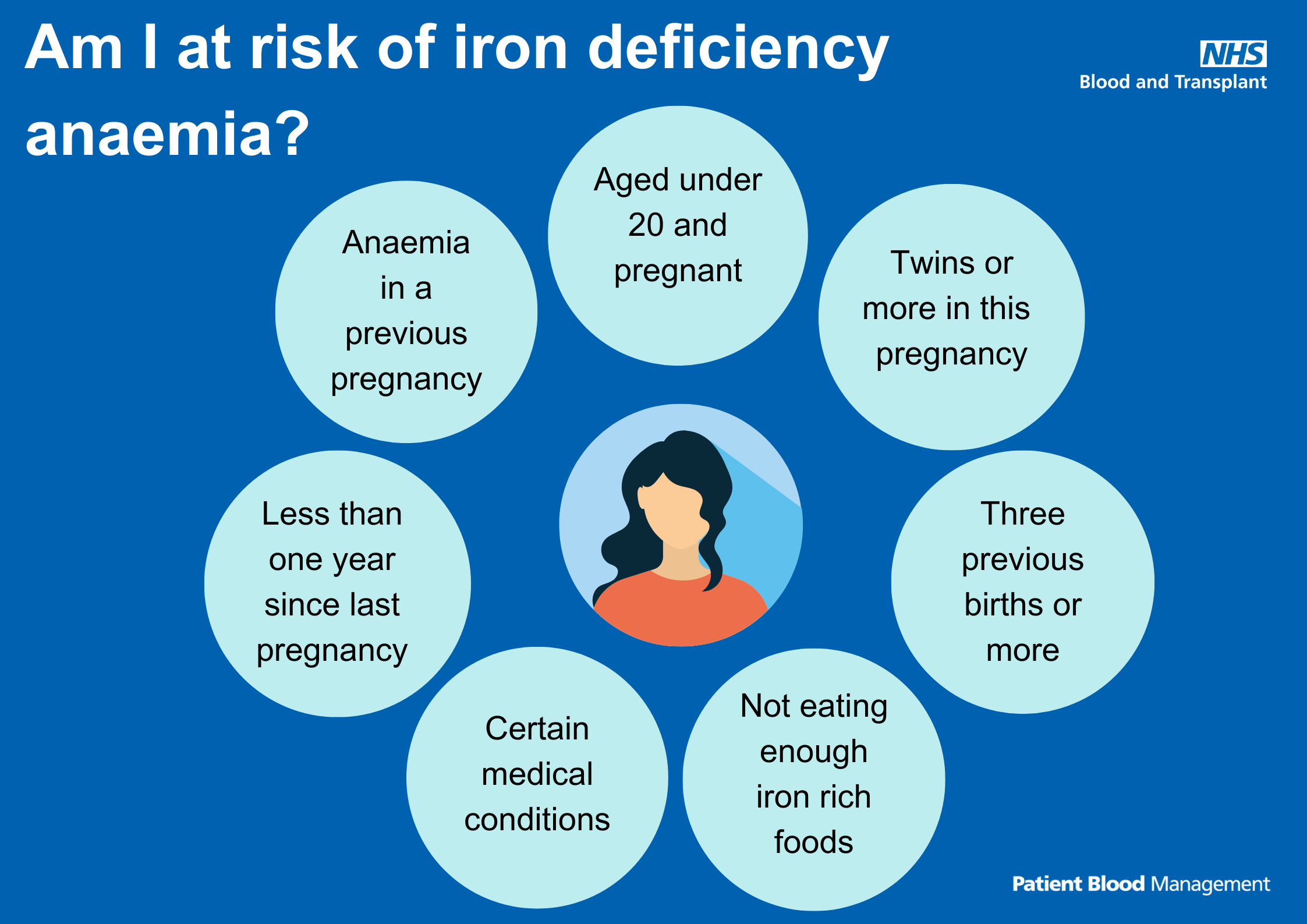
Text reads: "Am I at risk of iron deficiency anaemia?
- Aged under 20 and pregnant
- Twins or more in this pregnancy
- Three previous births or more
- Not eating enough iron rich foods
- Certain medical conditions
- Less than one year since last pregnancy
- Anaemia in a previous pregnancy"
Treating anaemia with iron tablets
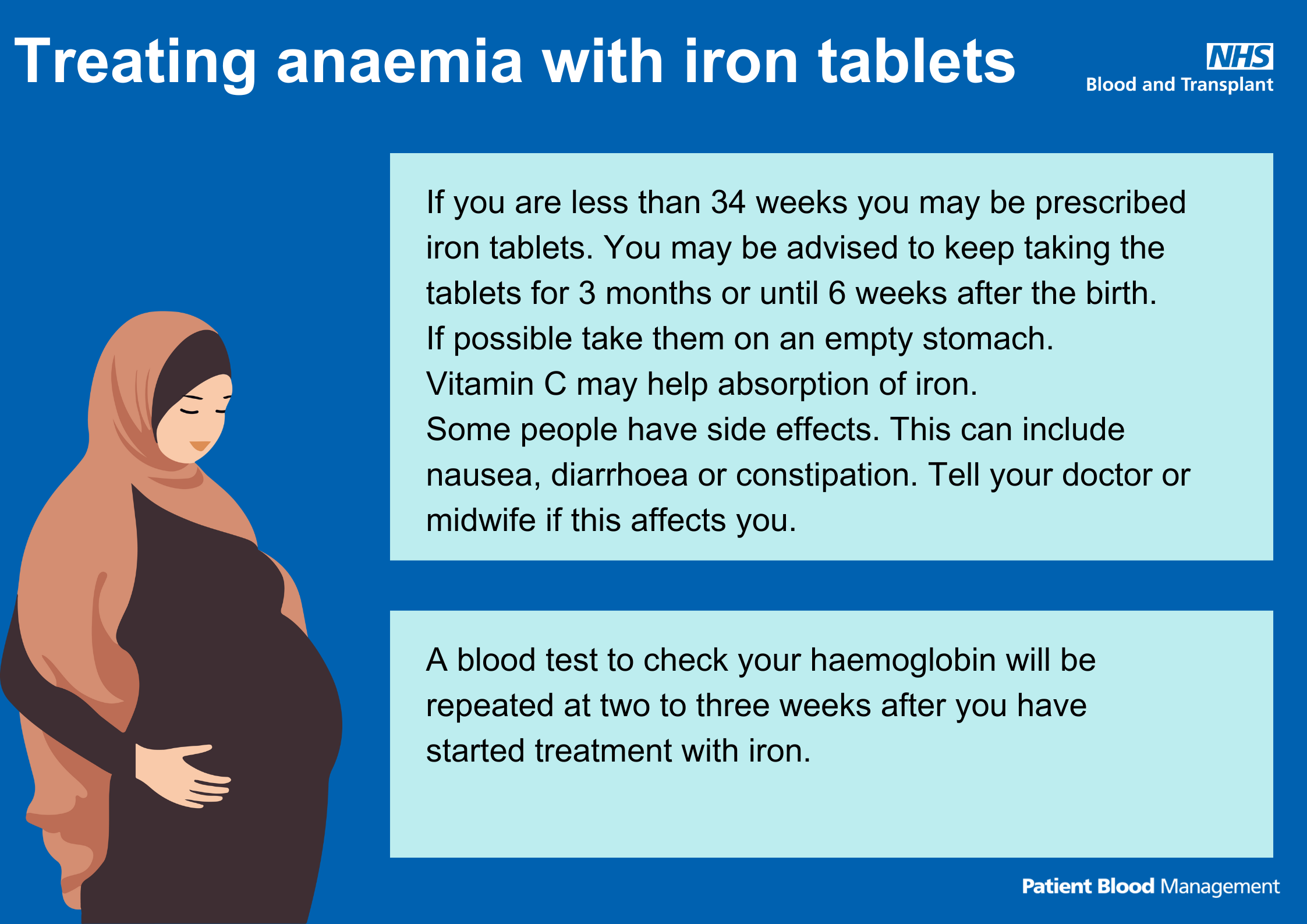
Text reads: "Treating anaemia with iron tablets.
If you are less than 34 weeks, you may be prescribed iron tablets. You may be advised to keep taking the tablets for 3 months or until 6 weeks after the birth.
If possible, take them on an empty stomach.
Vitamin C may help absorption of iron.
Some people have side effects. This can include nausea, diarrhoea, or constipation. Tell your doctor or midwife if this affects you.
A blood test to check your haemoglobin will be repeated at 2 to 3 weeks after you have started treatment with iron."
Treating anaemia with an iron infusion
Text reads: "Treating anaemia with an iron infusion.
If you are more than 34 weeks or anaemia is making you very unwell, you may receive an iron infusion into your veins. This usually takes place in the hospital and does not require an overnight stay.
A blood test to check your haemoglobin will be repeated at 2 to 3 weeks after you have started treatment with iron."
Share your learning
Tell us about your projects for obstetric anaemia, highlighting your successes or where things didn't go so well, and we'll include them on this page.
Contact us at pbm.team@nhsbt.nhs.uk
Page last reviewed: 10 February 2025
