Iatrogenic anaemia toolkit
This toolkit is for healthcare professionals to support the implementation of good practice within hospital and community settings to reduce iatrogenic anaemia (hospital-acquired anaemia).
In this section
Pages in the 'Identify and manage anaemia' section
What is iatrogenic anaemia?
Iatrogenic anaemia or hospital-acquired anaemia occurs when medical interventions, particularly blood sampling lead to anaemia. This can be as a result from repeated or frequent blood tests, including large amounts of blood samples taken over a period of time, even when clinically needed. It is frequently seen in patients who already have underlying health conditions.
The American Board of Internal Medicines' (ABIM) Choosing Wisely campaign urged healthcare professionals to question performing blood testing unless it was clinically indicated or necessary for diagnosis or patient care management purposes to avoid iatrogenic anaemia.
Anaemia caused by frequent blood sampling can lead to longer hospital stays and mortality, increased cost of consumables from laboratory testing, and subjects patients to unnecessary interventions.
Who is at risk of iatrogenic anaemia?
- Neonates and children, due to their low body weight
- Elderly people who have low body weight and, or, pre-existing anaemia
- Patients in intensive therapy units (ITUs) with pre-existing co-morbidities and potential anaemia
- Patients with underlying anaemia
- Patients who have bone marrow suppression
- Patients with blood loss and surgical blood loss
Infographics
These infographics are designed for you to use alongside appropriate text in presentations and educational resources. Please acknowledge the NHS Blood and Transplant Patient Blood Management team as the author.
What is iatrogenic anaemia?
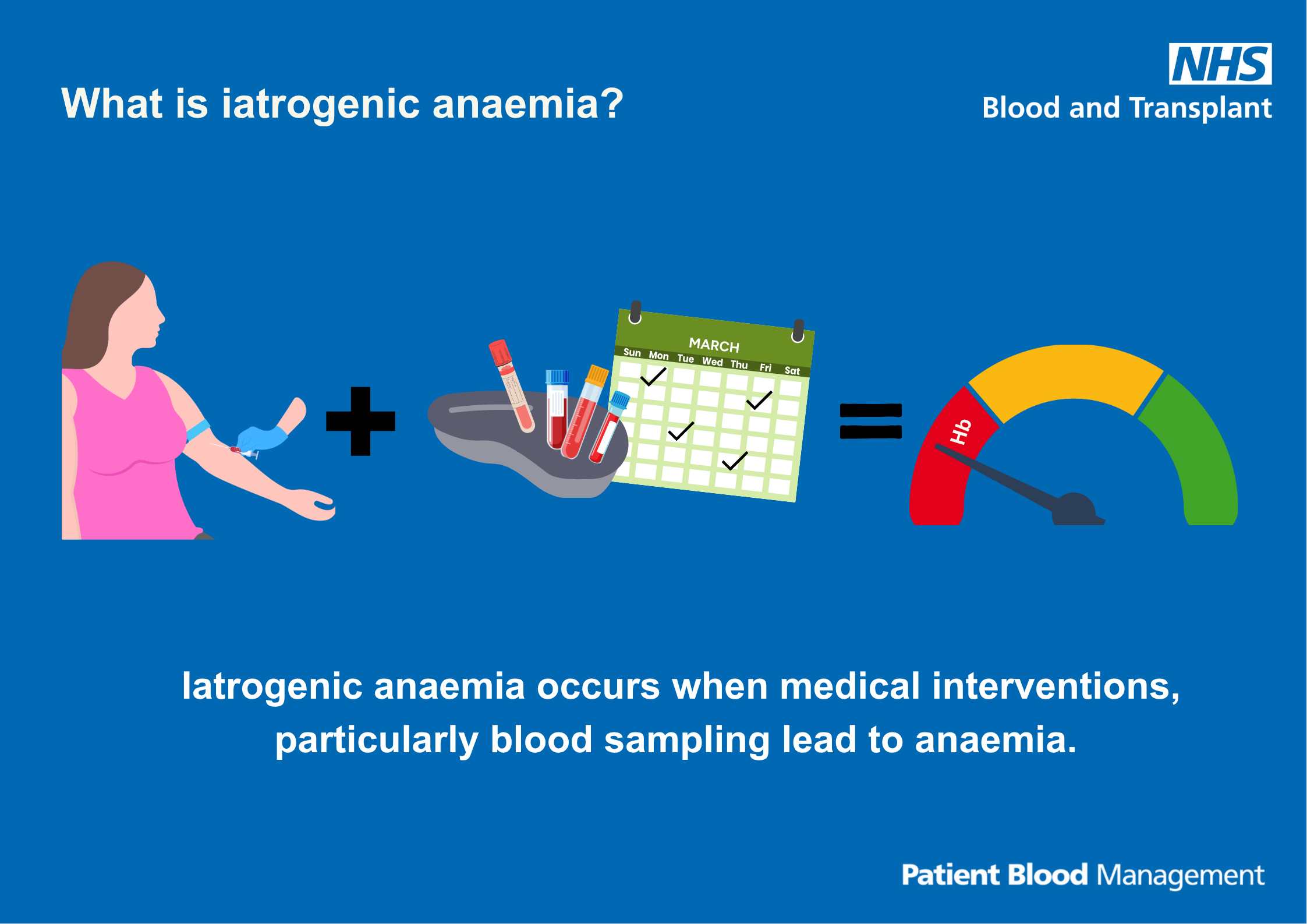
Text reads: "What is iatrogenic anaemia?
Iatrogenic anaemia occurs when medical interventions, particularly blood sampling lead to anaemia."
Download the infographic What is iatrogenic anaemia? (PDF 831KB)
Who is at risk of iatrogenic anaemia?
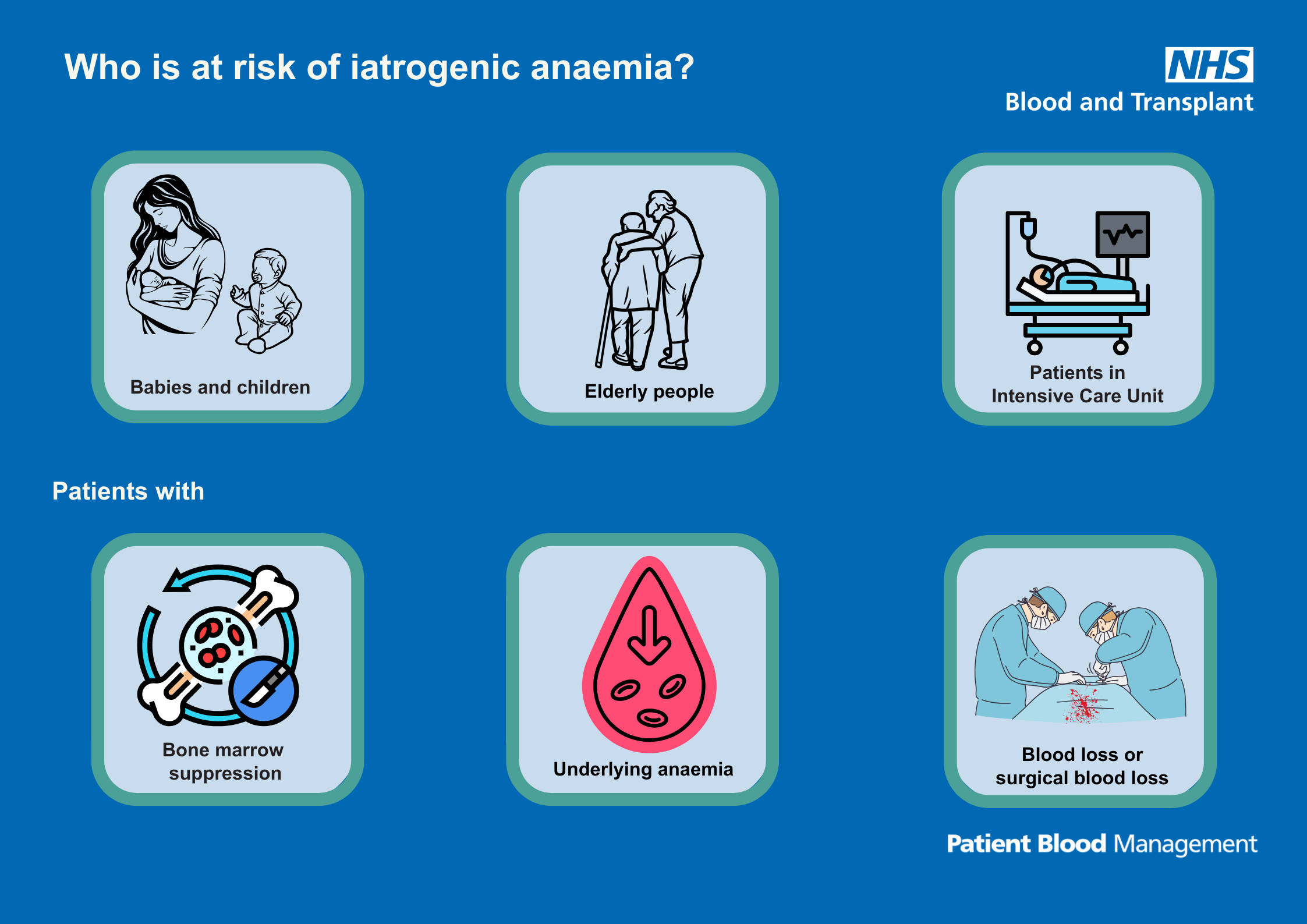
Text reads: "Who is at risk of iatrogenic anaemia?
Babies and children, elderly people, patients in intensive care units
Patients with bone marrow suppression, underlying anaemia, blood loss or surgical blood loss."
Download the infographic Who is at risk of iatrogenic anaemia? (PDF 284KB)
Unnecessary and rejected samples
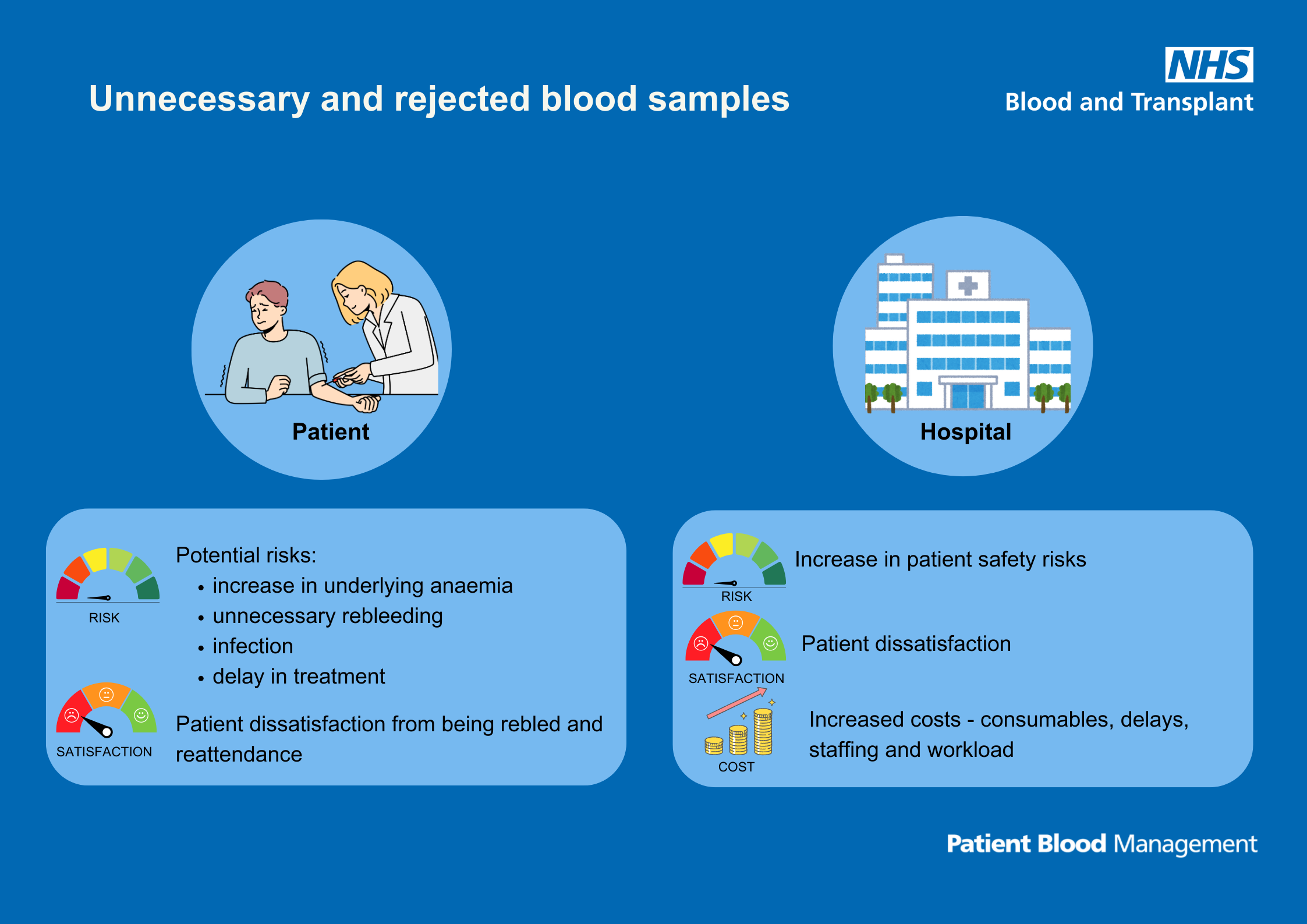
Text reads: "Unnecessary and rejected samples
Patient potential risks:
- Increase in underlying anaemia
- Unnecessary rebleeding
- Infection
- Delay in treatment
- Patient dissatisfaction from being rebled and reattendance
Hospital
- Increase in patient safely risks
- Patient dissatisfaction
- Increase costs – consumables, delays, staffing and workload."
Download the infographic Unnecessary and rejected samples (PDF 1175KB)
How to reduce blood sample rejection
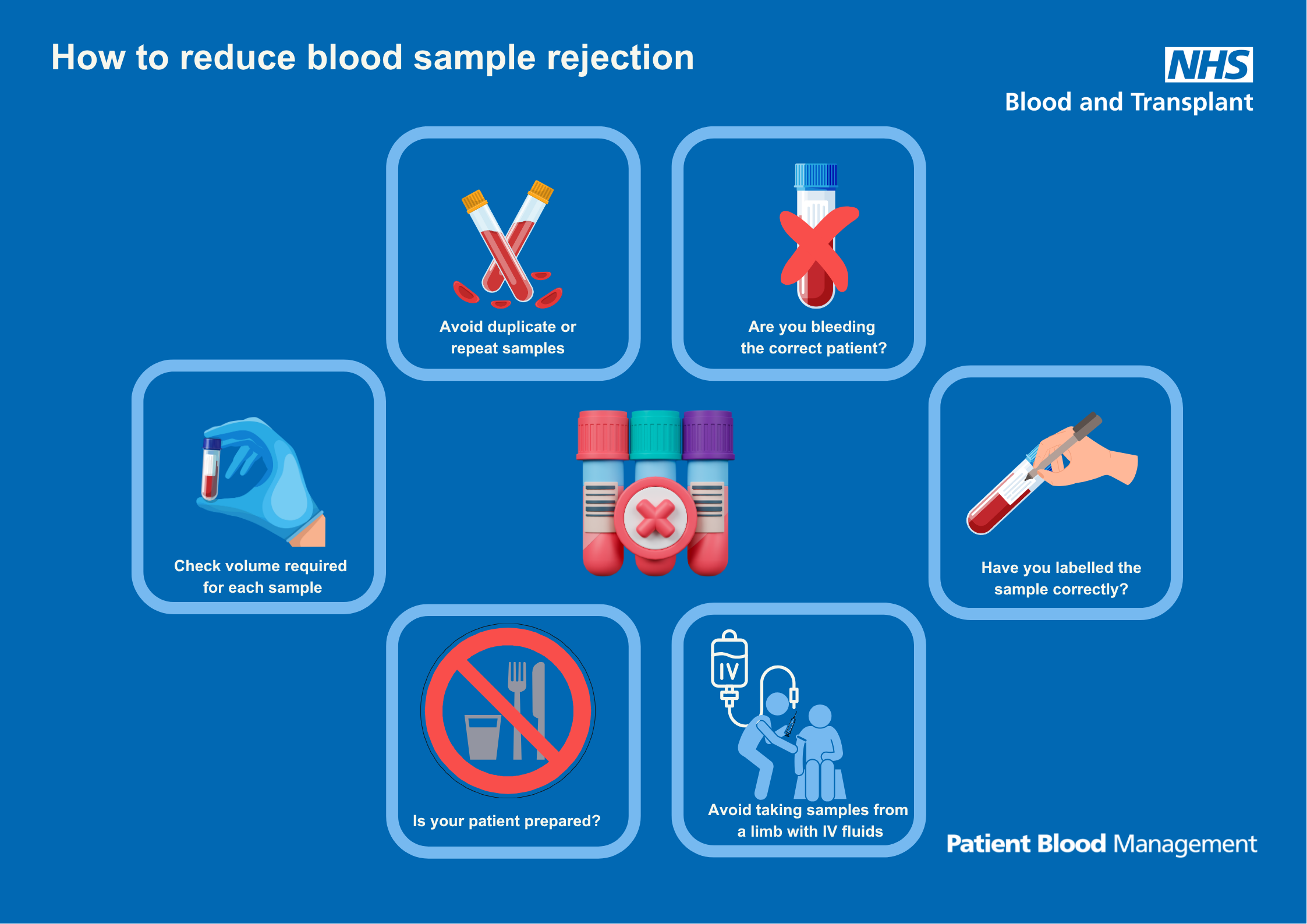
Text reads: "How to reduce blood sample rejection
- Avoid duplicate or repeat samples
- Are you bleeding the correct patient?
- Have you labelled the sample correctly?
- Avoid taking samples from a limb with IV fluids
- Is your patient prepared?
- Check volume required for each sample."
Download the infographic How to reduce blood sample rejection (PDF 835KB)
Clinical review may reduce blood sampling
Text reads: "Clinical review may reduce blood sampling
- Is my patient clinically stable?
- Has my patient had recent blood tests?
- Are there any underlying risks of anaemia?
- Will this test result change my patient’s care management?
Please refer to your hospital policy for minimum retesting guidance."
Download the infographic Clinical review may reduce blood sampling (PDF 797KB)
How can we prevent iatrogenic anaemia?
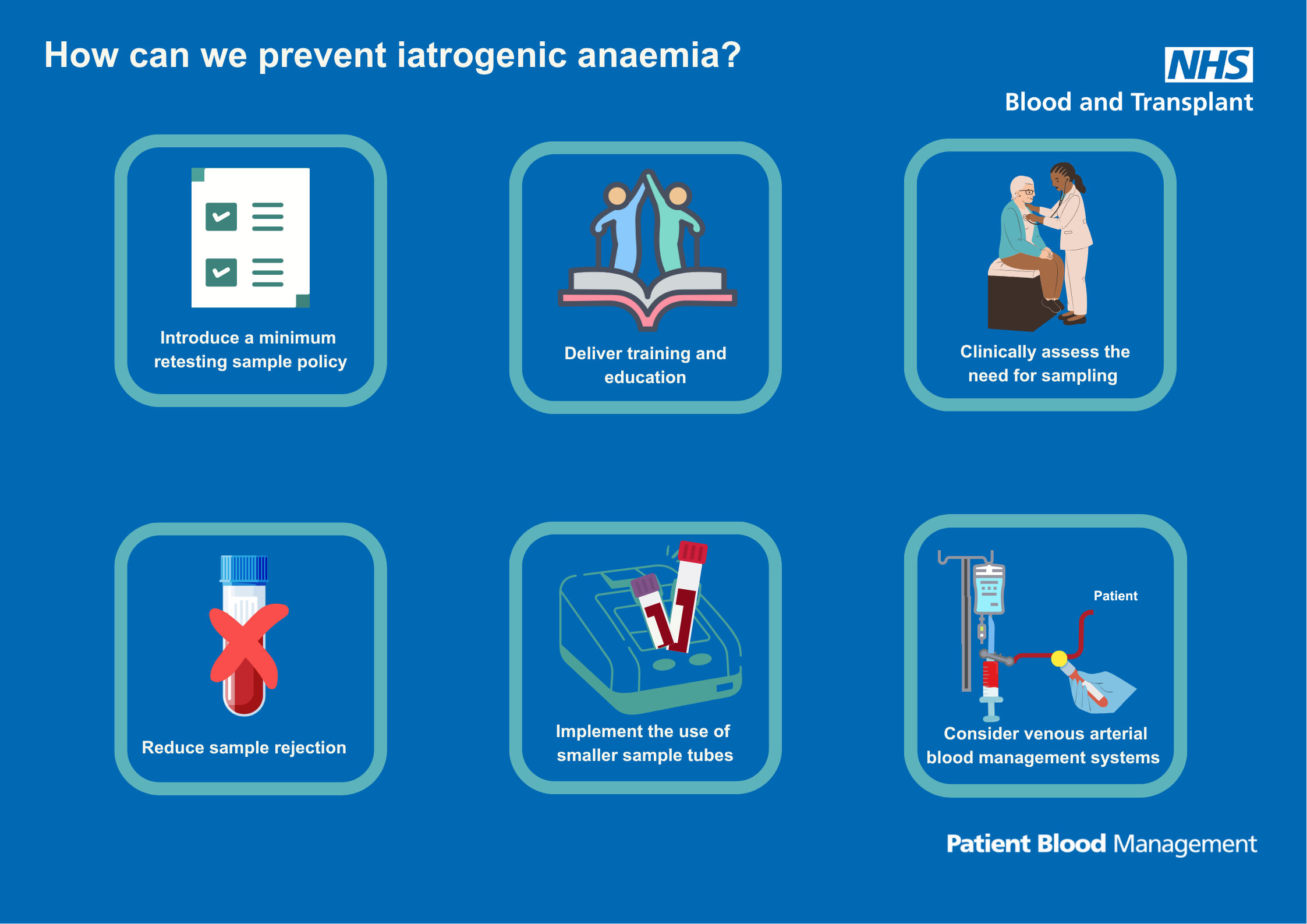
Text reads:"How can we prevent iatrogenic anaemia?
- Introduce a minimum retesting sample policy
- Deliver training and education
- Clinically assess the need for sampling
- Reduce sample rejection
- Implement the use of smaller sample tubes
- Consider venous arterial blood management systems."
Download the infographic How can we prevent iatrogenic anaemia? (PDF 1065KB
Share your learning
We are developing the content on this page and welcome your suggestions. Please send them to the team at: pbm.team@nhsbt.nhs.uk
Page last reviewed: 7 July 2025
