Single unit blood transfusions toolkit
This page contains information for clinical and laboratory transfusion staff to support a single unit approach to blood transfusion.
Patient blood management strategies are paramount to optimise patients' own red cells and avoid transfusion where possible.
However, where transfusion is unavoidable, restrictive haemoglobin thresholds and a single unit approach should be adopted. This means:
- transfusing one dose of blood component at a time in non-bleeding, stable patients
- clinical reassessment with a further blood count if necessary to determine future transfusion requirements
By transfusing one unit at a time, we can minimise inappropriate transfusion and reduce the risks associated with transfusion, such as Transfusion-Associated Circulatory Overload (TACO).
In this section
Pages in the 'Appropriate use of blood components' section
Infographics
These infographics are designed for you to use alongside appropriate text in presentations and educational resources. Please acknowledge the NHS Blood and Transplant Patient Blood Management team as the author.
Don't give two without review
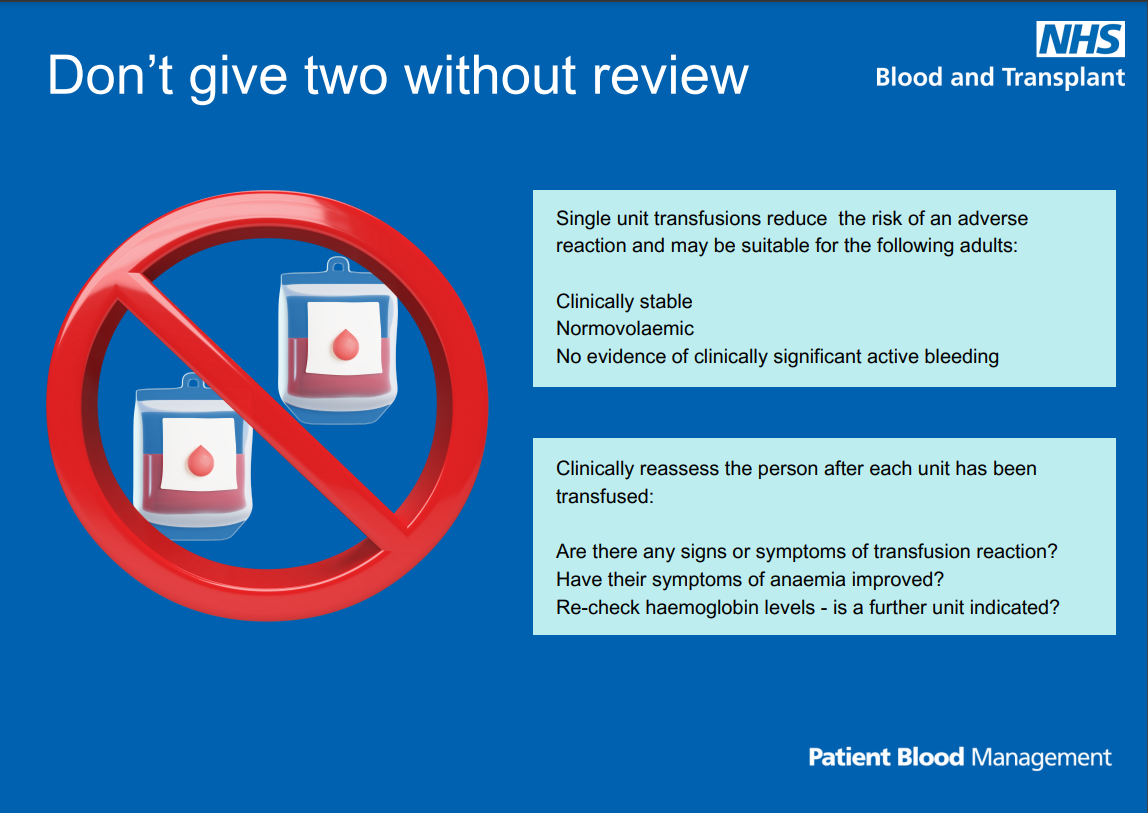
Text reads: "Single unit transfusions reduce the risk of an adverse reaction and may be suitable for the following adults:
- Clinically stable
- Normovolaemic
- No evidence of clinically significant active bleeding
Clinically reassess the person after each unit has been transfused:
- Are there any signs or symptoms of transfusion reaction?
- Have their symptoms of anaemia improved?
- Re-check haemoglobin levels - is a further unit indicated?"
Download the single unit transfusion infographic (PDF 1,041 KB)
Share your learning
Tell us about your single unit blood transfusions projects, highlighting your successes or where things didn't go so well, and we'll include them on this page.
Contact us at: pbm.team@nhsbt.nhs.uk
Page last reviewed: 10 February 2025
