Adults undergoing elective, scheduled surgery 2016
This was a re-audit of the audit performed in 2015. There has been an improvement in Patient Blood Management (PBM) practice since 2015.
Key aim
We re-audited surgical patients against 11 Patient Blood Management (PBM) algorithms, in preoperative (5) operative (2) and post-operative care settings (4).
Objectives
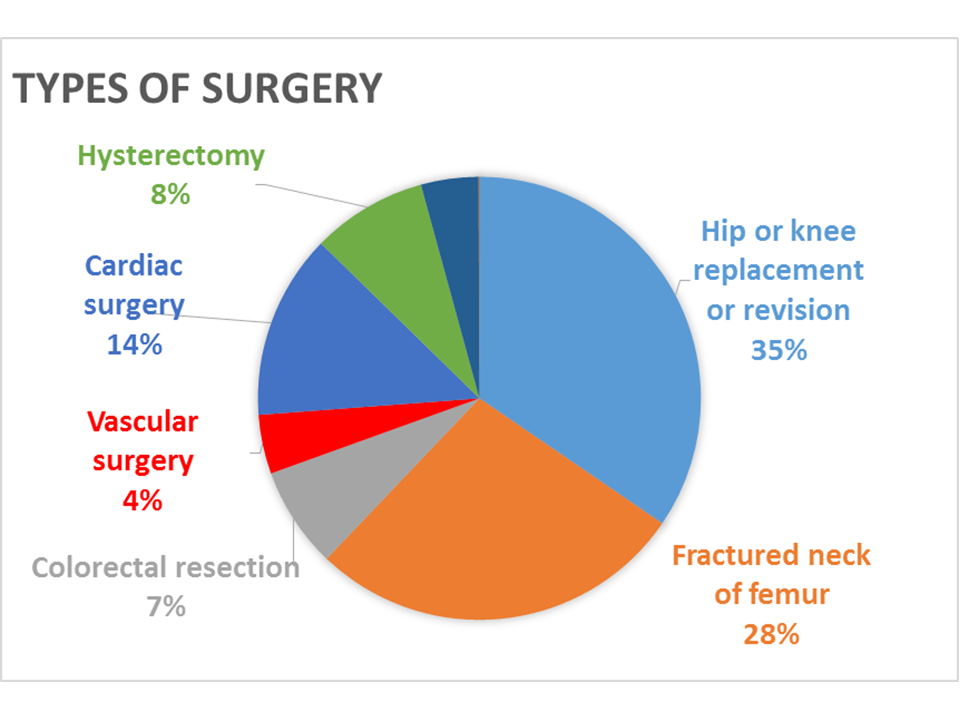
We re-audited elective procedures likely to be associated with high transfusion use including orthopaedic, cardiac, colorectal, urological, gynaecological and vascular surgery.
We also re-audited patients with a fractured neck of femur because they represent a large transfusion user group providing an opportunity to assess the scope for PBM measures in the urgent care setting, acknowledging that pre-operative management is often impractical.
Who took part
We audited 3266 patients from156 sites over 3 months (September to November) in 2016. 138 hospitals also participated in the 2015 audit (data from 2015 are based on these 138 hospitals).
What did we find?
Preoperative (excluding fractured neck of femur)
In those patients having elective surgery 50% (1175/2361) received appropriate pre-operative anaemia management before surgery (PBM 1). This is an improvement in practice from 2015.
A pre-operative transfusion was prescribed in 4.3% (102/2362) patients. Only 15% (14/90) were prescribed when the Hb was less than the defined threshold for transfusion (PBM 2).
Preoperative (including fractured neck of femur)
The single unit transfusion approach was followed by clinical staff in 34% (62/186) of patients (PBM 4). This is probably an improvement in practice from 2015.
Operative
Clinical staff attempted at least oneappropriate PBM measure in 81% (572/704) of patients undergoing major blood loss surgery who received an intra-operative transfusion (PBM 6a).
Clinical staff attempted all appropriate PBM measures in 20% (141/705) of patients undergoing major blood loss surgery who received an intra-operative transfusion (PBM 7a).
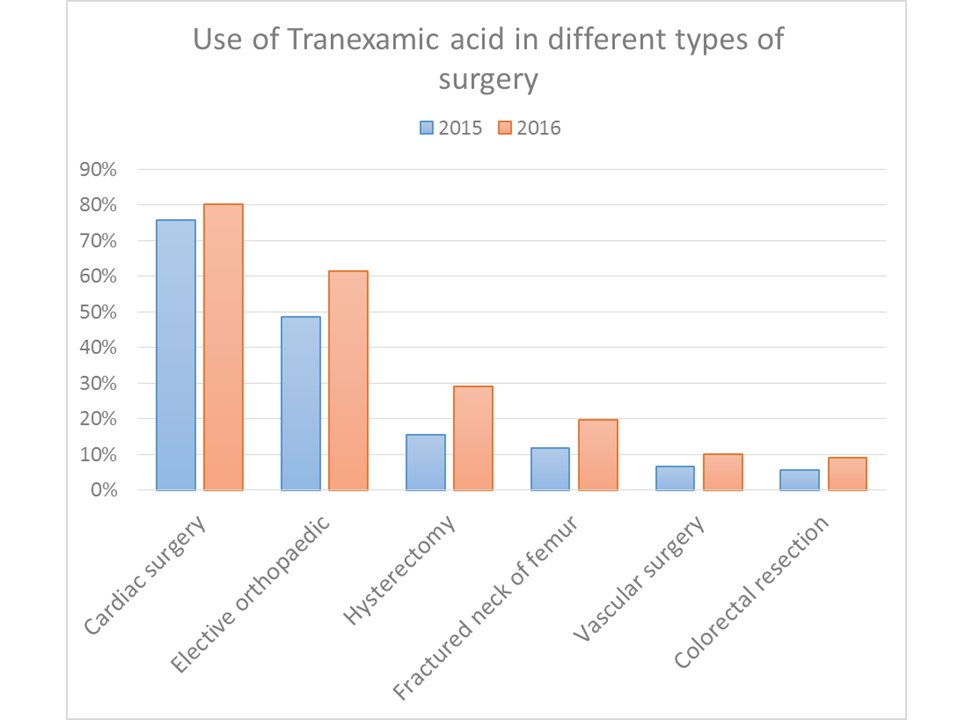
Tranexamic acid was used in 42% (1367/3255) of patients. This is an improvement in practice from 2015.
Cell salvage was collected in 17% (539/3261) of cases and re-infused in 87% (468/537). There was little change in the use of cell salvage between 2015 and 2016.
Post operative
In patients without active bleeding a transfusion was prescribed when the Hb was less than the defined threshold in 34% (797/2356) of patients (PBM 8). This is an improvement in practice from 2015.
The single unit transfusion approach was followed by clinical staff in 49% (903/1825) of patients (PBM 9). This is an improvement in practice from 2015.
Clinical staff attempted at least one appropriate PBM measure in 84% (1404/1672) of patients undergoing major blood loss surgery who received their first post-operative transfusion (PBM 10a).
Clinical staff attempted all appropriate PBM measures in 10% (172/1668) of patients undergoing major blood loss surgery who received their first post-operative transfusion (PBM 11a). This is an improvement in practice from 2015.
Resources to help improve practice
Please cite this document as:
The PBM in Elective Surgery Working Group on behalf of the National Comparative Audit of Blood Transfusion. 'The 2016 Patient Blood Management in adults undergoing elective, scheduled surgery' (2017). https://doi.org/10.71745/j3w5-5h32
