2018 Audit of the management of major haemorrhage
Key objectives
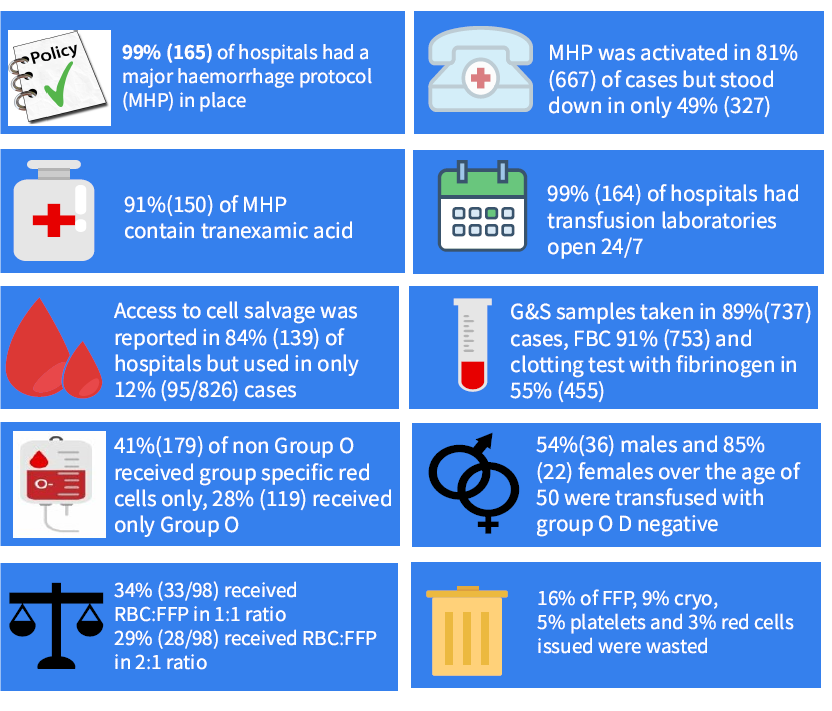
• Determine transfusion laboratory infrastructure for supporting and delivering the major haemorrhage protocol in Trusts/Hospitals
• Evaluate different standards for management of major haemorrhage cases against existing national guidelines and understand how blood components are utilised in this situation with regards to issuing, usage and wastage.
What did we audit?
• Each hospital was asked to report up to 10 adult cases who were treated for major haemorrhages for any medical or surgical reason in October 2018
• We looked at blood component use, time taken to obtain blood components, amount of blood component wastage and use of other methods to manage blood loss
Who took part?
What did we find?
Organisational recommendations
• All hospitals should ensure that tranexamic acid is part of MHP.
• All hospitals should perform regular annual drills of their MHP systems to ensure that all mechanisms for contacting relevant members involved with delivering blood components to patients are co-ordinated well and that all clinical teams involved with MHP are trained to implement these protocols effectively.
• Clinical and laboratory teams should ensure that MHPs are audited regularly to monitor and minimise blood wastage.
• Pre-thawed FFP can be considered by major trauma centres and hospitals with high FFP usage in order to reduce wastage.
• Clinical teams must be trained to recognize major blood loss early, and to know when to activate and stand down the major haemorrhage protocol.
• Tranexamic acid (unless contraindicated) should be given to all patients with major bleeding.
• Intra-operative cell salvage should be used in relevant high blood loss procedures.
• Clinical staff should ensure that Group & Save samples are taken during major haemorrhage to allow for transfusion of group specific RBCs as soon as possible, so group O red cells are reserved for extreme emergency.
• Clotting screens including fibrinogen should be taken during major haemorrhage to allow for guided transfusion.
• For management of major bleeding where patient’s blood group is unknown, Group O D negative red cells should be use for females of child bearing age (<50 years old) and group O D positive red cells for males and women >50 years old.
• Trauma patients should receive a 1:1 ratio of RBC to FFP continuously for the management of bleeding.
Please cite this document as:
Green and others on behalf of the National Comparative Audit of Blood Transfusion. '2018 Audit of the Management of Major Haemorrhage' (2019). https://doi.org/10.71745/rgsg-p674
