Red blood cell transfusion in hospices 2016
Aims
- Determine current practice regarding red blood cell transfusion in palliative hospice care
- Compare practice against NICE and BSH guidelines on blood transfusion
- Develop recommendations to improve practice
What did we audit?
- All red blood cell transfusions over a 3 month period starting in September or October 2016
Who took part?
- 121 hospices took part, 107 in England, 9 in Scotland, 2 in Wales and 1 in Northern Ireland
- Organisational audit: 54 hospices
- Clinical audit:
- 121 hospices, 38 hospices did not perform a transfusion during the 3 month period
- 465 patients
What did we find?
- Full report (PDF)
Organisational audit
96% (52/54) had local written transfusion guidelines. However, only 9% (5/54) mentioned the need to weigh patients prior to transfusion.
Clinical audit
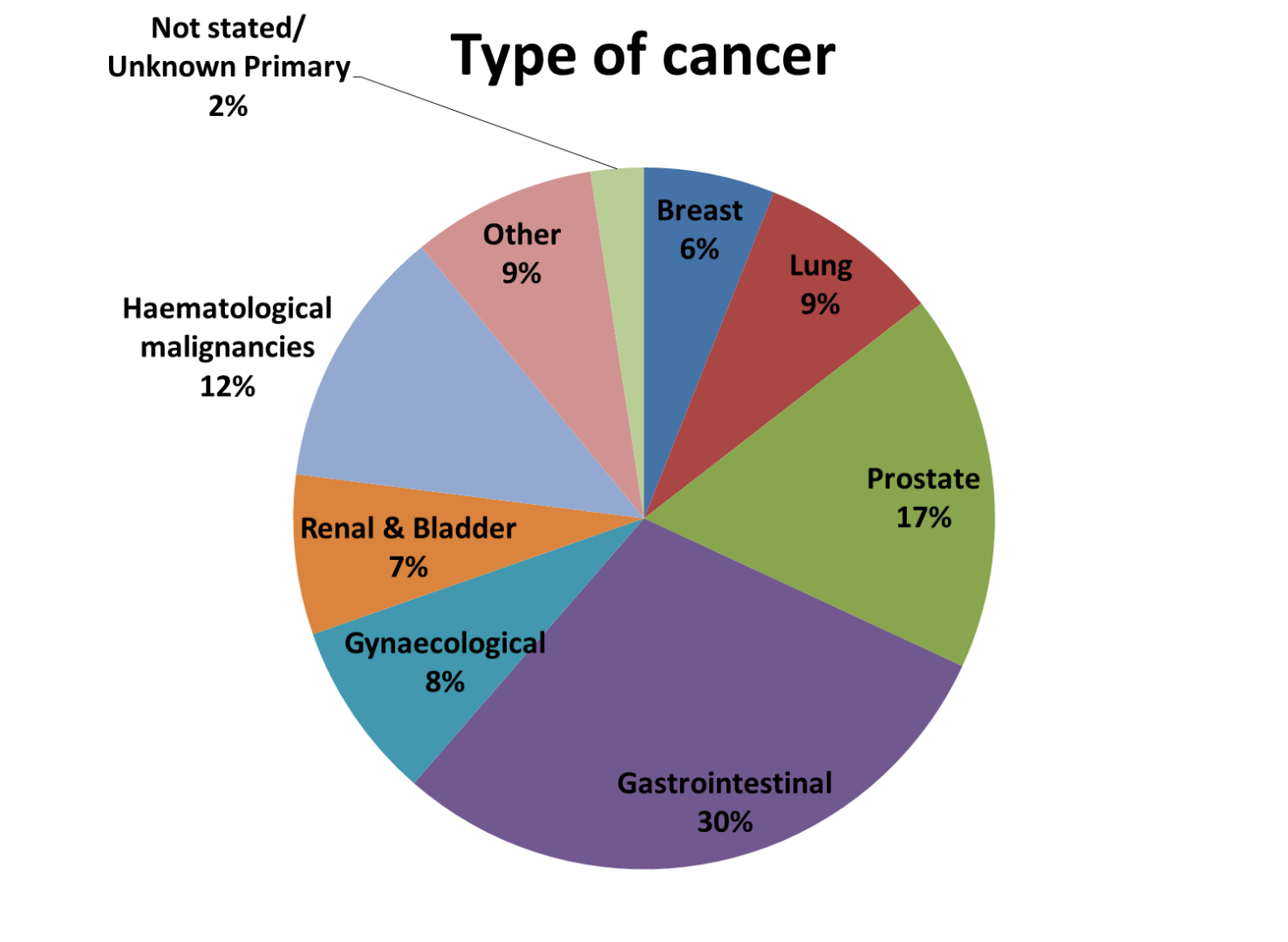
465 patients received a red cell transfusion. 96% (448/465) had an underlying diagnosis of cancer. 39% (181/465) had an expected life-expectancy of more than 3 months.
Prior to transfusion
29% (137/465) had haematinics checked. 76 had iron deficiency or functional iron deficiency. 12 may have benefited from B12 injections, and 41 may have benefited from folic acid.
91% (422/465) had consented to the transfusion, but only 71% (332/465) had risks and benefits of transfusion explained.
Only 15% (68/465) had a weight known prior to transfusion.
During the transfusion
86% (400/465) of patients had their observations checked before, during and after the first unit of the transfusion.
5% (25/465) of patients had a haemoglobin level check after every unit transfused. Only two patients went on to have a second red cell unit after their Hb level was checked.
Only 16% (75/465) of patients had a single red cell unit.
After the transfusion
Fewer than 1 in 5 patients derived a sustained benefit from the transfusion, as assessed by a clinician or performance status.
Although only 15% (68/465) of patients who received a transfusion had been expected to die within 4 weeks, 32% (150/465) had died within 30 days of the red cell transfusion.
To help improve practice
Please cite this document as:
The Red Blood Cell Transfusion in Hospices Working Group on behalf of the National Comparative Audit of Blood Transfusion. '2016 National Comparative Audit of Red Blood Cell Transfusion in Hospices' (2017). https://doi.org/10.71745/6kmp-r242
Publications
- Estcourt, L., Gray, R. & Neoh, K. (2017) UK-wide audit of red blood cell transfusion in hospices. Vox Sanguinis, 112, 71.
- Grant-Casey, J., Gray, R., Boland, J. & Estcourt, L. (2017) The use of red cells in hospice-based palliative medicine. Vox Sanguinis, 112, 262.
- Neoh, K., Gray, R., Malia, C., Estcourt, L. & Boland, J.W. (2017) 2016 National comparative audit of red blood cell transfusion in hospices. BMJ Supportive & Palliative Care, 7, A19-20.
